Navigating Cataract Surgery with Diabetes: Essential Tips for a Successful Outcome
- Dr. Jakhar Healthcare

- 1 day ago
- 3 min read
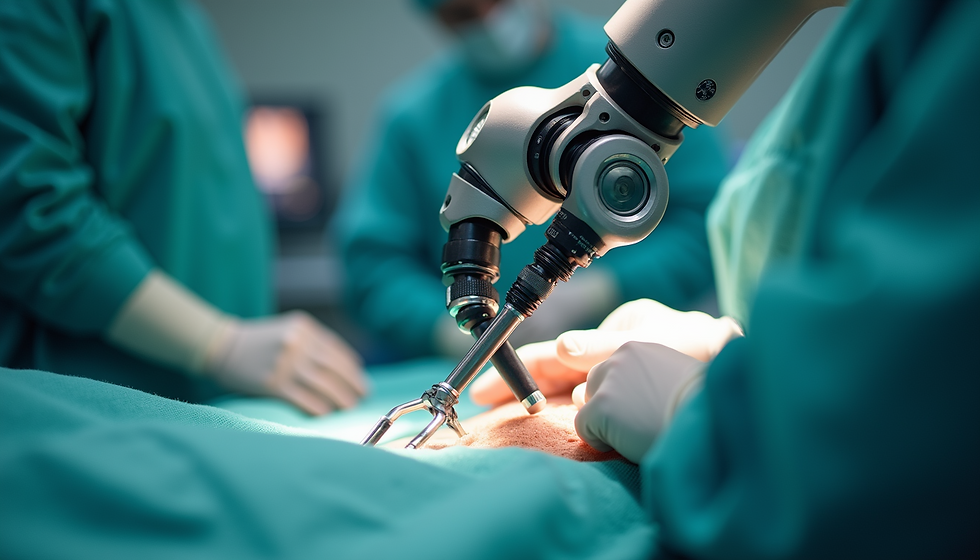
Managing diabetes while preparing for cataract surgery requires careful planning and attention. Diabetes affects many parts of the body, including the eyes, and can complicate surgical procedures. For individuals with diabetes, cataract surgery is not just a routine operation. It demands extra care to ensure the best possible results and to avoid complications. Understanding the challenges and steps involved can help patients feel more confident and prepared for their surgery.

Assessing the Situation Before Surgery
Diabetes can cause changes in the eyes that affect surgery outcomes. One common condition is Diabetic Retinopathy (DR), where high blood sugar damages the tiny blood vessels in the retina. If DR is present or advanced, it can increase the risk of complications during and after cataract surgery.
Before scheduling surgery, doctors perform thorough eye exams to check the retina’s health. This may include:
Dilated eye exams to see the retina clearly
Optical coherence tomography (OCT) scans to detect swelling or damage
Fluorescein angiography to assess blood vessel leakage
These tests help the surgeon understand the risks and plan the procedure carefully. If diabetic retinopathy is detected, treatment such as laser therapy or injections may be needed before cataract surgery.
Maintaining stable blood sugar levels is critical. High glucose levels can worsen eye conditions and slow healing. Patients should work closely with their endocrinologist or primary care physician to keep diabetes under control before surgery.
Preparation for Surgery
Proper preparation can reduce risks and improve recovery. Here are key steps diabetic patients should follow before cataract surgery:
Manage blood glucose levels
Keep blood sugar within the target range. Fluctuations can increase the chance of infection and delay healing. Monitoring levels daily and adjusting diet or medication as advised is essential.
Inform your doctor about medications
Some diabetes medications like metformin or SGLT2 inhibitors may require adjustments before surgery. Always disclose all medications to your surgeon and healthcare team.
Follow pre-surgery instructions carefully
Your eye surgeon will provide specific guidelines, such as fasting before surgery or using prescribed eye drops. Following these instructions reduces complications.
Discuss other health issues
Diabetes often affects the heart, kidneys, and nerves. Inform your doctor about any related problems, as these can influence anesthesia and recovery.
Avoid certain substances and activities
Stop taking aspirin or blood thinners if advised, as they can increase bleeding risk. Also, avoid makeup, lotions, or creams on the face on the day of surgery to reduce infection risk.
Preparing mentally is also important. Understanding the procedure, expected outcomes, and recovery process helps reduce anxiety and promotes cooperation with post-surgery care.

Post-Surgery Care
Recovery after cataract surgery requires ongoing attention, especially for people with diabetes. The healing process may take longer, and the risk of complications is higher if blood sugar is not well controlled.
Key post-surgery care tips include:
Monitor blood sugar regularly
Stress and reduced physical activity after surgery can cause blood sugar spikes. Frequent monitoring helps catch and manage these changes early.
Follow medication and eye drop schedules
Use all prescribed eye drops to prevent infection and inflammation. Missing doses can lead to complications.
Attend all follow-up appointments
Regular check-ups allow the surgeon to monitor healing and detect any issues early, such as infection or increased eye pressure.
Watch for warning signs
Contact your doctor immediately if you notice increased pain, redness, vision changes, or discharge from the eye.
Be patient with healing
Healing times vary, but diabetic patients may experience slower recovery. Avoid strenuous activities and protect your eyes from dust and bright light.
Maintain overall health
Continue managing diabetes, blood pressure, and other health conditions. Good overall health supports eye healing.

Understanding the Risks and Benefits
Cataract surgery can significantly improve vision and quality of life. For diabetic patients, the benefits often outweigh the risks when proper care is taken. However, diabetes increases the chance of complications such as:
Delayed healing
Infection
Swelling of the retina (macular edema)
Worsening of diabetic retinopathy
By controlling blood sugar and following medical advice, many patients experience successful surgery and improved vision.
Final Thoughts
Managing diabetes during cataract surgery requires a team approach involving the patient, eye surgeon, and diabetes care providers. Careful assessment, preparation, and follow-up are essential to reduce risks and support healing. If you have diabetes and are scheduled for cataract surgery, start by discussing your condition openly with your healthcare team. Keep your blood sugar stable, follow all medical instructions, and attend all appointments.



Comments